Author: Dr Vaibhav Singh, King George’s Medical University
Reference: Harrison’s Principles of Internal Medicine, 21st Edition

Definition: SBP>130 & DBP>80 mmHg
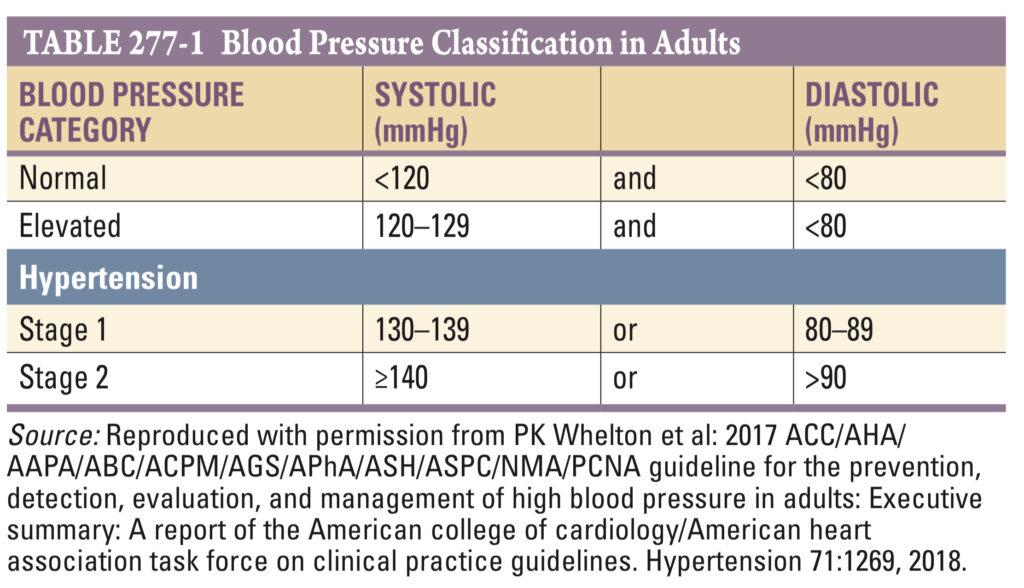
-In children & adolescents: HTN is SBP and/or DBP consistently >95th percentile for age, sex, and height.
–Prehypertensive: BP between the 90-95 percentiles, requires lifestyle interventions.
-Home BP & 24-h ambulatory BP measurements are generally lower than clinic BP.
-BP tends to be higher in the early morning hours, soon after waking, than at other times of day. MI & stroke are more common in the early morning hours. Night-time BP are generally 10–20% lower than daytime BP, and an attenuated night-time blood pressure “dip” is associated with increased cardiovascular disease risk.
White coat HTN: elevated office blood pressures but normal 24 hr ambulatory readings.(15–20%)
Masked HTN: Opposite of White coat HTN (Normal office blood pressures but elevated 24 hr ambulatory readings)
Primary (Essential) Hypertension
80-95% HTN cases are essential or idiopathic, with no specific cause (including patients with obesity & metabolic syndrome).
Characteristics: familial, influenced by genetics and environment, and increases with age.
Pathophysiology: Typically, patients show increased peripheral resistance and normal or decreased cardiac output. However, in younger patients with mild HTN, cardiac output may be increased and peripheral resistance may be normal.
Plasma Renin Activity (PRA): In hypertensive patients, 10-15% have high PRA (vasoconstrictor form of HTN) and 25% have low PRA (volume-dependent HTN).
Obesity and HTN: Association exists between obesity(BMI>30), especially with central fat distribution, and HTN.
Metabolic Syndrome: HTN with dyslipidaemia and insulin resistance, & abdominal obesity.
This increases risks for coronary heart disease, stroke, and diabetes.
Insulin Resistance: About 25-50% of nonobese, nondiabetic hypertensive individuals are insulin resistant. Insulin resistance and hyperinsulinemia(surrogate marker of insulin resistance) are common in 1st degree relatives of 10 HTN and may predict HTN and cardiovascular disease.
Secondary Hypertension
HTN due to any underlying cause. (5-20% cases)
Suspect 20 HTN if there are: Characteristic clinical features, severe or drug-resistant HTN, recent onset HTN, disproportionate TOD, and younger age.
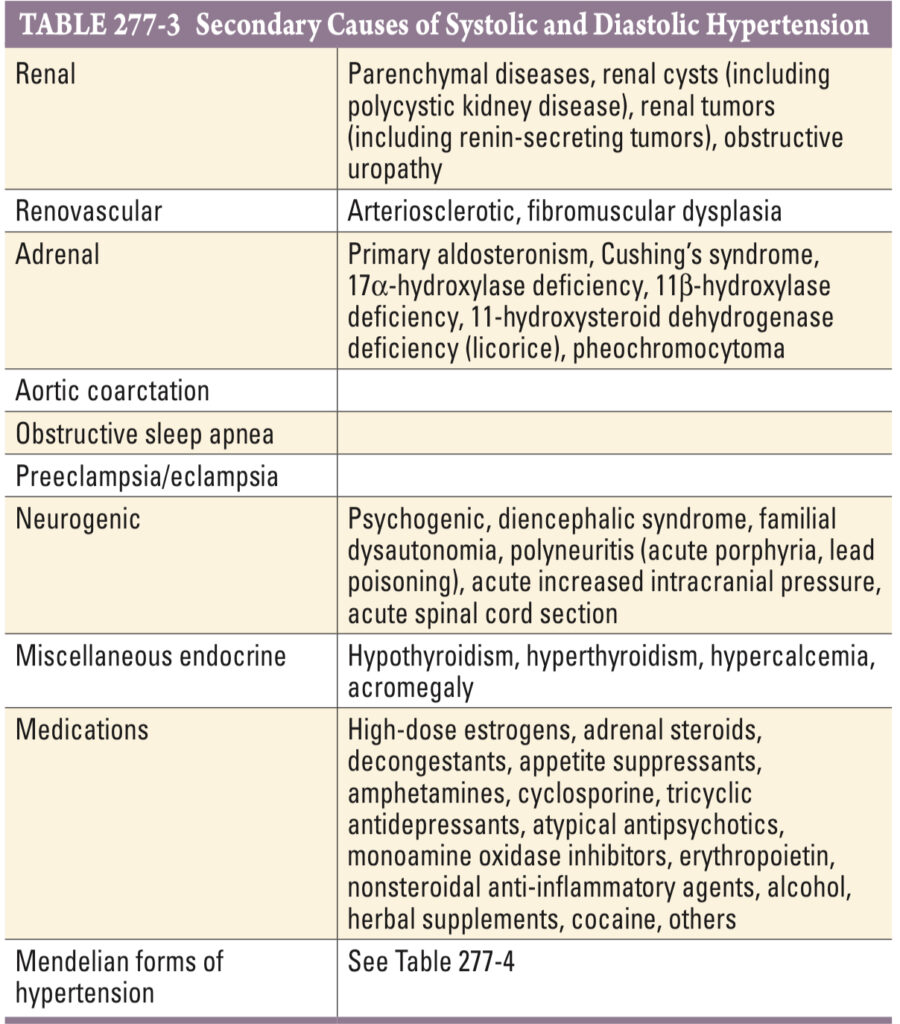
Renal Parenchymal Disease: Renal disease is the most common cause of secondary HTN. HTN is present in >80% of patients with chronic renal failure. Conversely, HTN may cause nephrosclerosis, & in some instances, it may be difficult to determine whether HTN or renal disease was the initial disorder.
Renovascular HTN
- Cause: Narrowing of the renal arteries, leading to high blood pressure.
- Initial Mechanism: RAAS Activation
- Over Time: Transient elevation in renin; sodium retention and other mechanisms contribute.
- Risk Groups:
- atherosclerosis (plaque in renal artery)- Older patients
- fibromuscular dysplasia– Younger patients(young white women). In contrast to atherosclerotic renovascular disease, it is usually B/L & affects more distal portions of the renal artery.
- Common Type in Fibromuscular Dysplasia: Medial Fibroplasia.
- Indicators of Renovascular HTN:
- Severe or refractory hypertension
- the recent loss of hypertension control
- carotid or femoral artery bruits
- flash pulmonary edema
- unexplained deterioration of renal function
- deterioration of renal function associated with an ACE inhibitor
- Symptom: Abdominal or flank bruit(50% of cases)
- Functionally Significant Lesion: >70% obstruction of the renal artery’s lumen.
- Investigations:
- Doppler USG
- Angiography (false negative in obese patients): Collateral vessels suggest significant lesions.
- Gd enhanced MRI (easily picks lesions in proximal parts of the renal artery but may miss distal lesions)
- Contrast arteriography (Gold Standard)
- Treatment:
- ACE inhibitors or ARB (risk of reduced kidney function in stenotic kidneys)
- Fibromuscular Disease: PTRA(Percutaneous Transluminal Renal Angioplasty) & stenting, Surgical renal revascularization.
Primary Aldosteronism
Cause: 90% cases-Aldosterone producing adenoma(usually unilateral, <3 cm diameter) & B/L adrenal hyperplasia
Remainder cases are due to B/L adrenocortical hyperplasia
Rare causes include adrenal carcinoma or ectopic malignancies.
Effects: Sodium retention, hypertension, hypokalemia, low PRA, Cardiovascular disease, & Renal damage
Diagnosis:
- Age: 3rd – 5th decades.
- Often associated with mild to moderate, sometimes severe, hypertension.
- Consider in refractory hypertension cases.
- Symptoms like polyuria, polydipsia, paresthesias, muscle weakness due to hypokalemic alkalosis may occur.
- High prevalence(40-50%) in hypertensive patients with unprovoked hypokalemia.
Screening Tests:
- Serum potassium levels (insensitive and nonspecific test).
- Plasma aldosterone to plasma renin activity (PA/PRA) ratio: a ratio >30:1 with PA >555 pmol/L (>20 ng/dL) indicates aldosterone-producing adenoma.
Problems in Testing:
- The cutoff for a “high” PA/PRA ratio varies depending on the laboratory.
- ACEI may increase renin & Aldosterone antagonists may increase aldosterone. So Withdraw the aldosterone antagonist for at least 4 weeks before testing PA.
- Aldosterone synthesis is potassium dependent so hypokalemia should be corrected before screening.
- In Renal insufficiency, PA/PRA ratio will be increased due to decreased clearance of aldosterone.
Confirmatory Tests: (Done when PA/PRA ratio is high)
- Failure to suppress plasma aldosterone after IV saline infusion, oral NaCl intake, fludrocortisone, or captopril.
Diagnosis and Differentiation:
- Adrenal CT: to identify tumors.
- Adrenal Scintigraphy: if CT is non-diagnostic
- B/L Adrenal venous sampling: to differentiate between U/L & B/L causes.
Treatment:
Laparoscopic Surgery (U/L adrenalectomy): for adenoma
Medical treatment: for bilateral hyperplasia or unsuitable surgical candidates of adenoma.
Postoperative monitoring for hypoaldosteronism.
Special Case: Glucocorticoid-Remediable Hyperaldosteronism:
- early-age severe hypertension.
- Family history of hemorrhagic stroke at a young age.
- Normally, angiotensin II stimulates aldosterone production by the adrenal zona glomerulosa, whereas ACTH stimulates cortisol production in the zona fasciculata.
- Due to a chimeric gene on chromosome 8, ACTH regulates aldosterone secretion in the zona fasciculata so there is high aldosterone and hybrid steroids (18-hydroxycortisol and 18-oxocortisol) due to oxidation of cortisol.
- Diagnosis: urine excretion rates of hybrid steroids or genetic testing.
- Treatment: low-dose glucocorticoids or spironolactone.
Approach
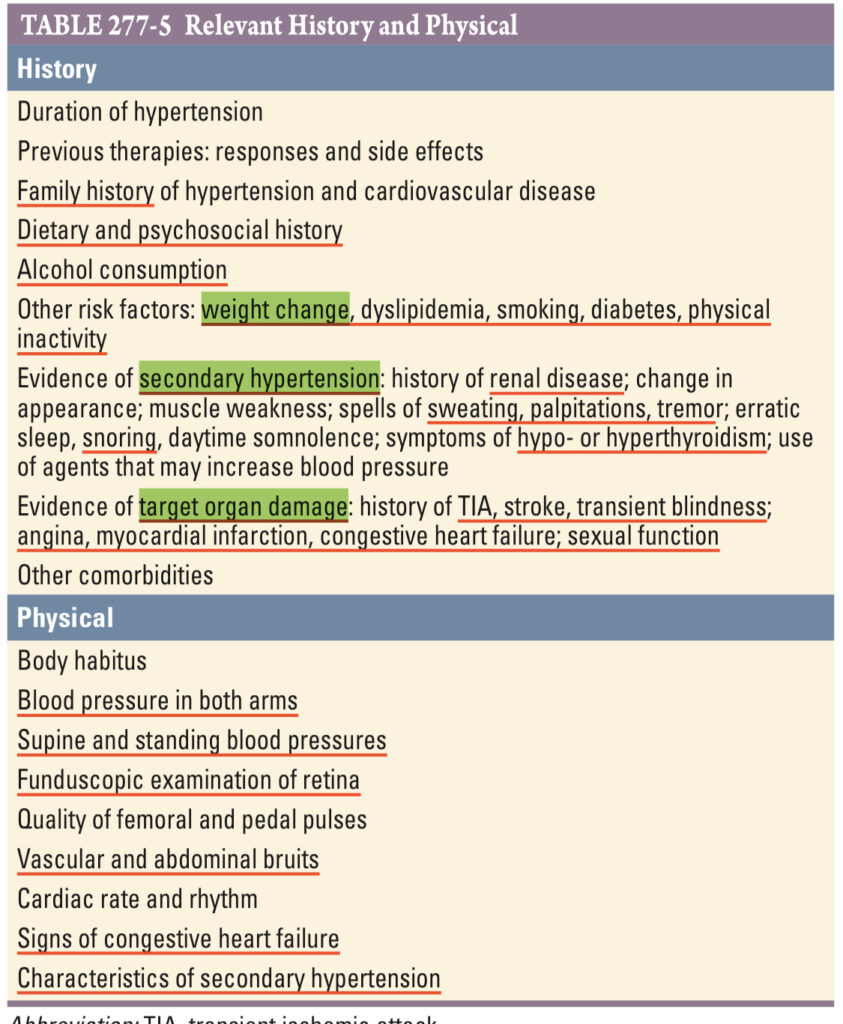
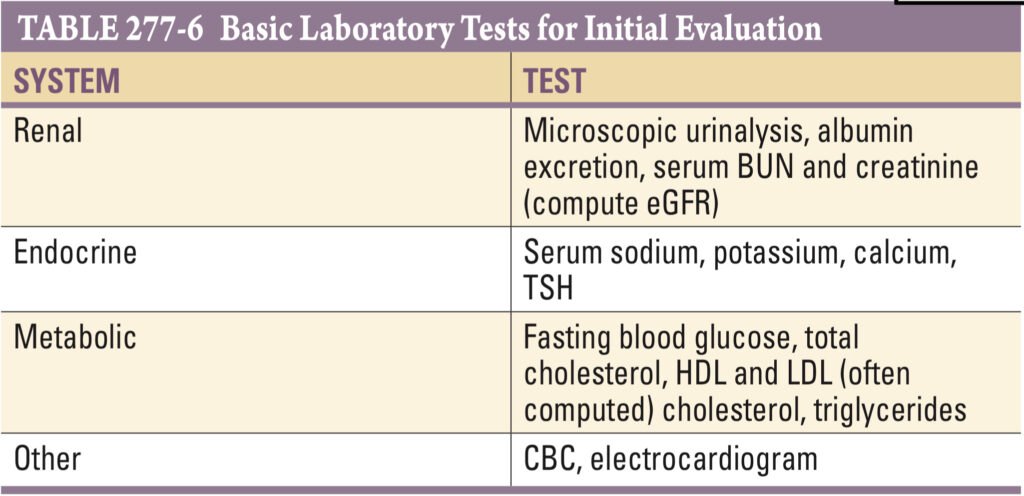
BP Measurement
Before the measurement, the patient should be seated quietly in a chair (not the exam table) with feet on the floor for 5 min in a private, quiet setting with a comfortable room temperature. At least two measurements should be made.
Cuff:
- The centre of the cuff should be at the heart level
- cuff width: at least 40% of the arm circumference
- length of the cuff bladder: enough to encircle at least 80% of the arm circumference.
- Rate of deflation of the cuff: 2 mmHg/s
- Systolic BP: first of at least two regular “tapping” Korotkoff sounds
- DBP: the point at which the last regular Korotkoff sound is heard
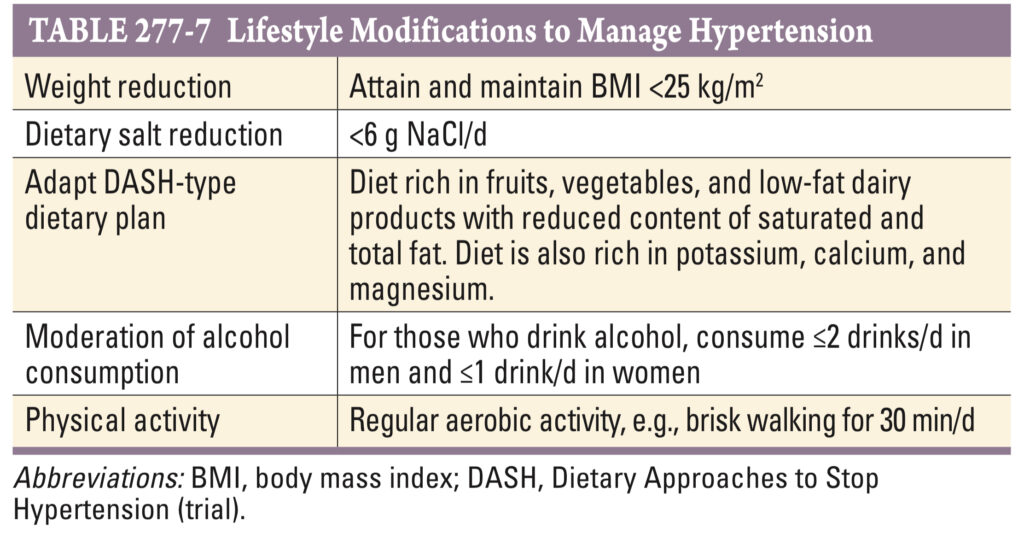
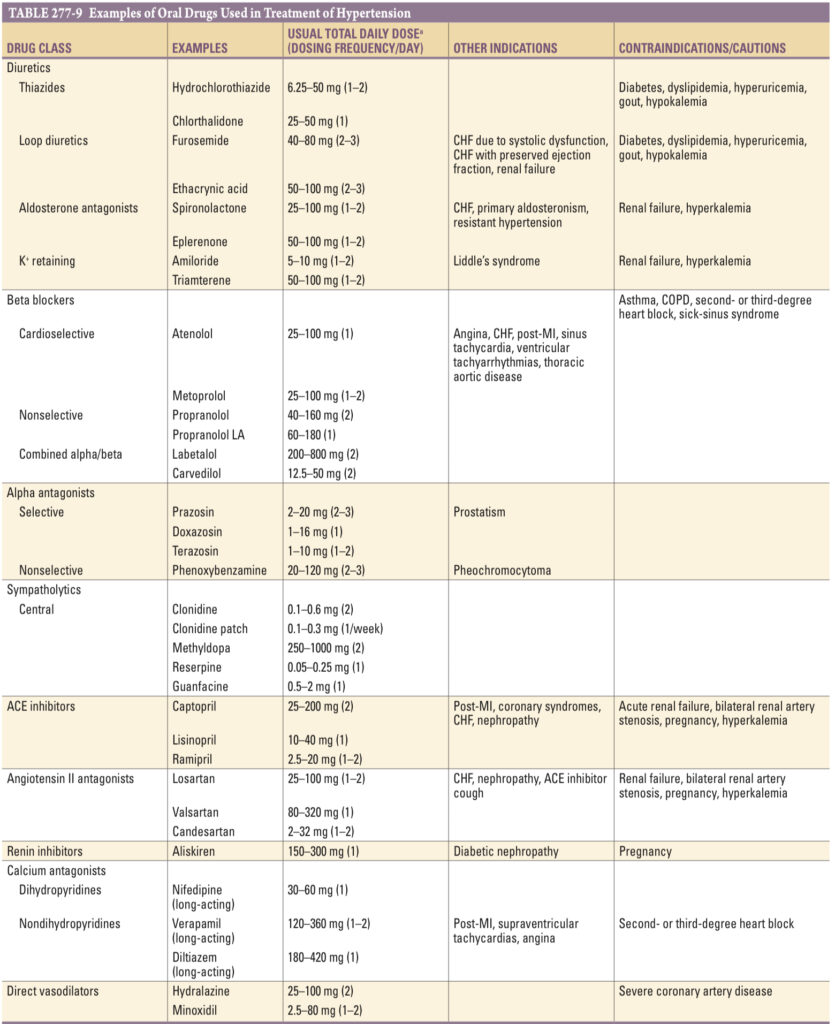
Management
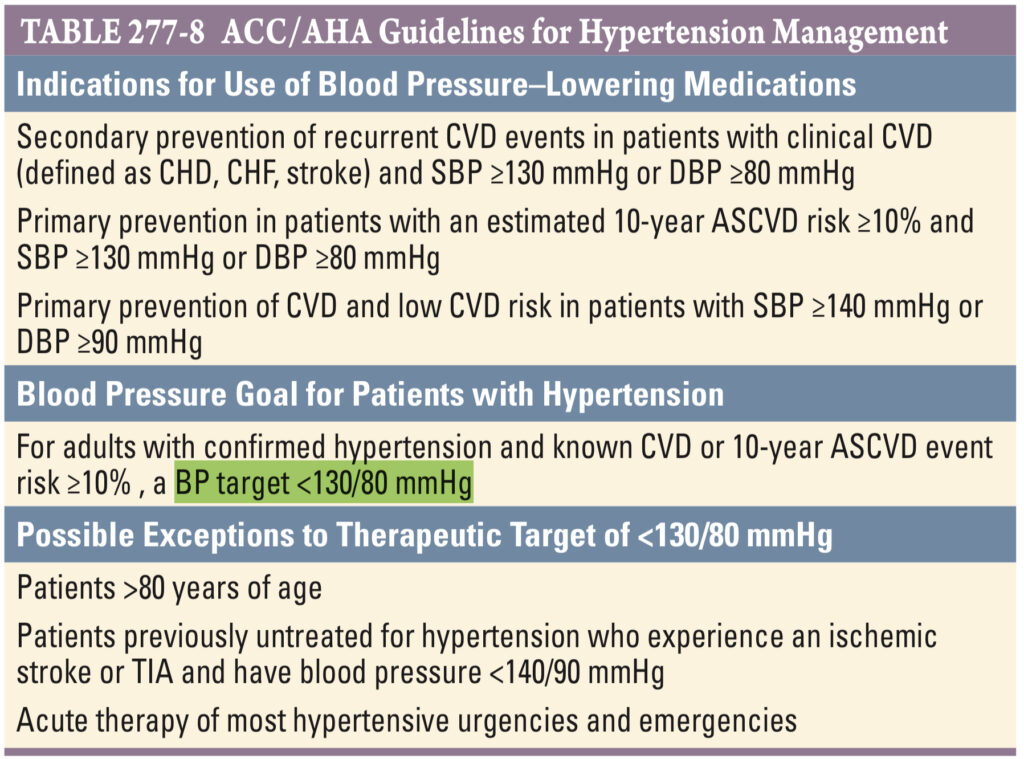
ACC/AHA recommends the goal of BP control as <130/80 mmHg for the primary and secondary prevention of cardiovascular disease including in patients with DM & CKD.
Resistant HTN
Definition: BP >140/90 mmHg despite using 3 or more antihypertensives, including a diuretic.
Prevalence: More common in patients over 60 years
Causes:
- Nonadherence
- Identifiable causes (obesity, Primary aldosteronism & excessive alcohol intake)
- Interference by nonprescription and prescription drugs.
Pseudohypertension in Older Patients: Rare occurrence due to severely sclerotic arteries, suggested if the radial pulse is palpable when the brachial artery is occluded (Osler maneuver).
Evaluation Approach:
- Home BP monitoring to verify if office readings are accurate.
- Evaluation for secondary HTN if no clear cause of resistance is identified.
Treatment: Spironolactone
Hypertensive Urgency / Emergency
Hypertensive Urgency: Severe asymptomatic HTN without acute target organ damage.
Management: Gradual lowering of BP over 24 hours to 25% of the initial BP. (Except in acute aortic dissections or hemorrhagic strokes)
Hypertensive Emergency: Severe HTN with acute target organ damage.
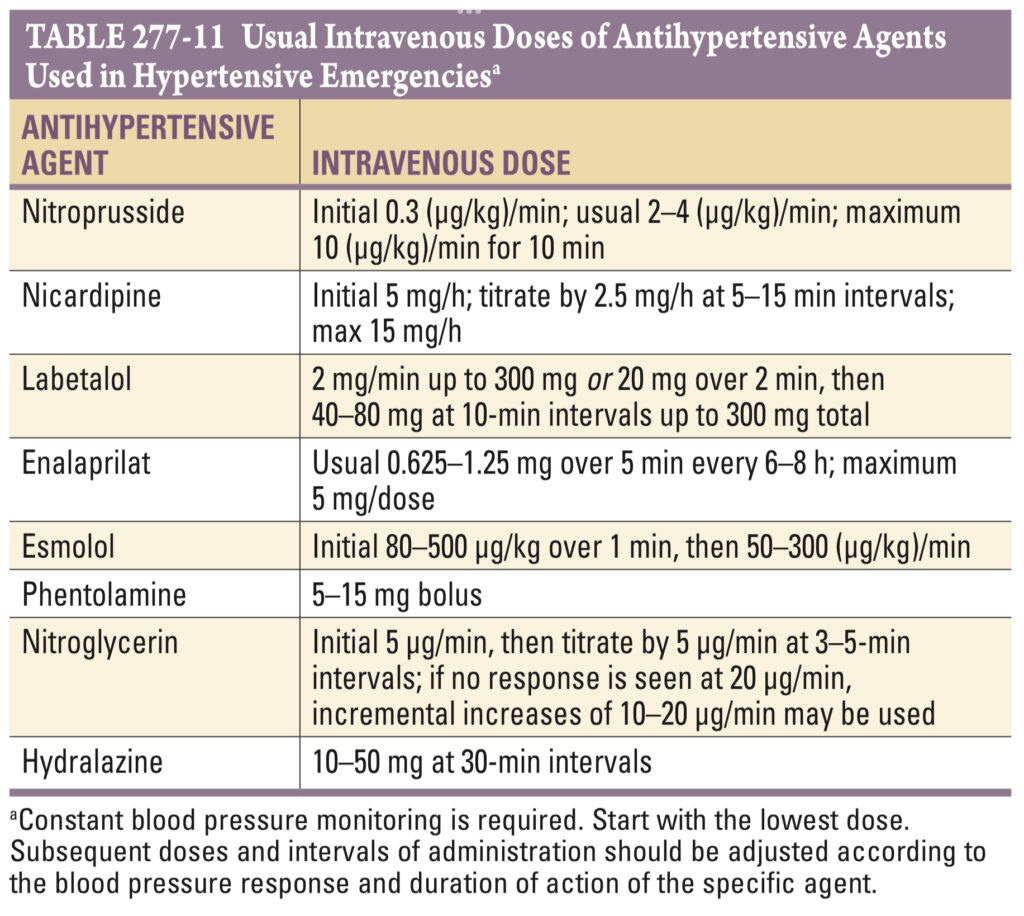
Treatment:
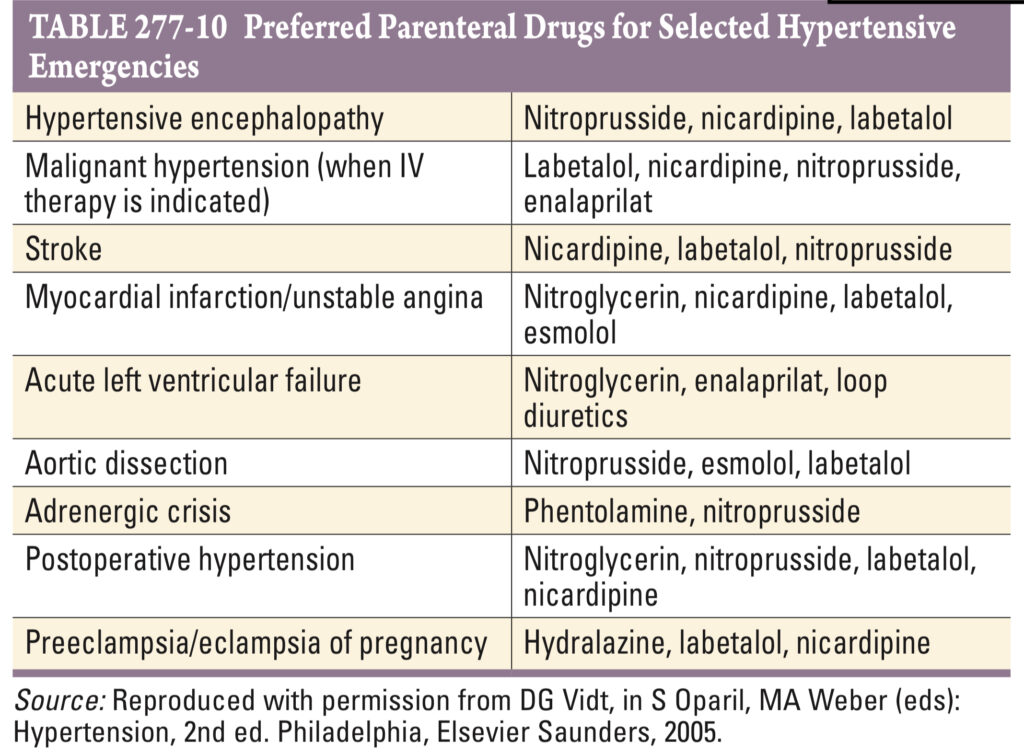
Malignant Hypertension
Abrupt increase in BP, significant for its rate instead of absolute BP level.
Pathology:
- Associated with diffuse necrotizing vasculitis.
- Presence of arteriolar thrombi.
- Fibrinoid necrosis: in arterioles of the kidney, brain, retina, & other organs.
Clinical Features:
- Progressive retinopathy, including arteriolar spasms, haemorrhages, exudates, and papilledema.
- Deteriorating renal function with proteinuria.
- Microangiopathic hemolytic anemia.
- Encephalopathy.
History: ask about the use of MAO inhibitors & drugs like cocaine and amphetamines.
Initial Treatment Goals in Encephalopathy Cases:
- Reduce mean arterial blood pressure by no more than 25% within minutes to 2 hours.
- Target blood pressure range: 160/100–110 mmHg.
Treatment Option: IV nitroprusside



